cervical cancer is a treatable, preventable disease.
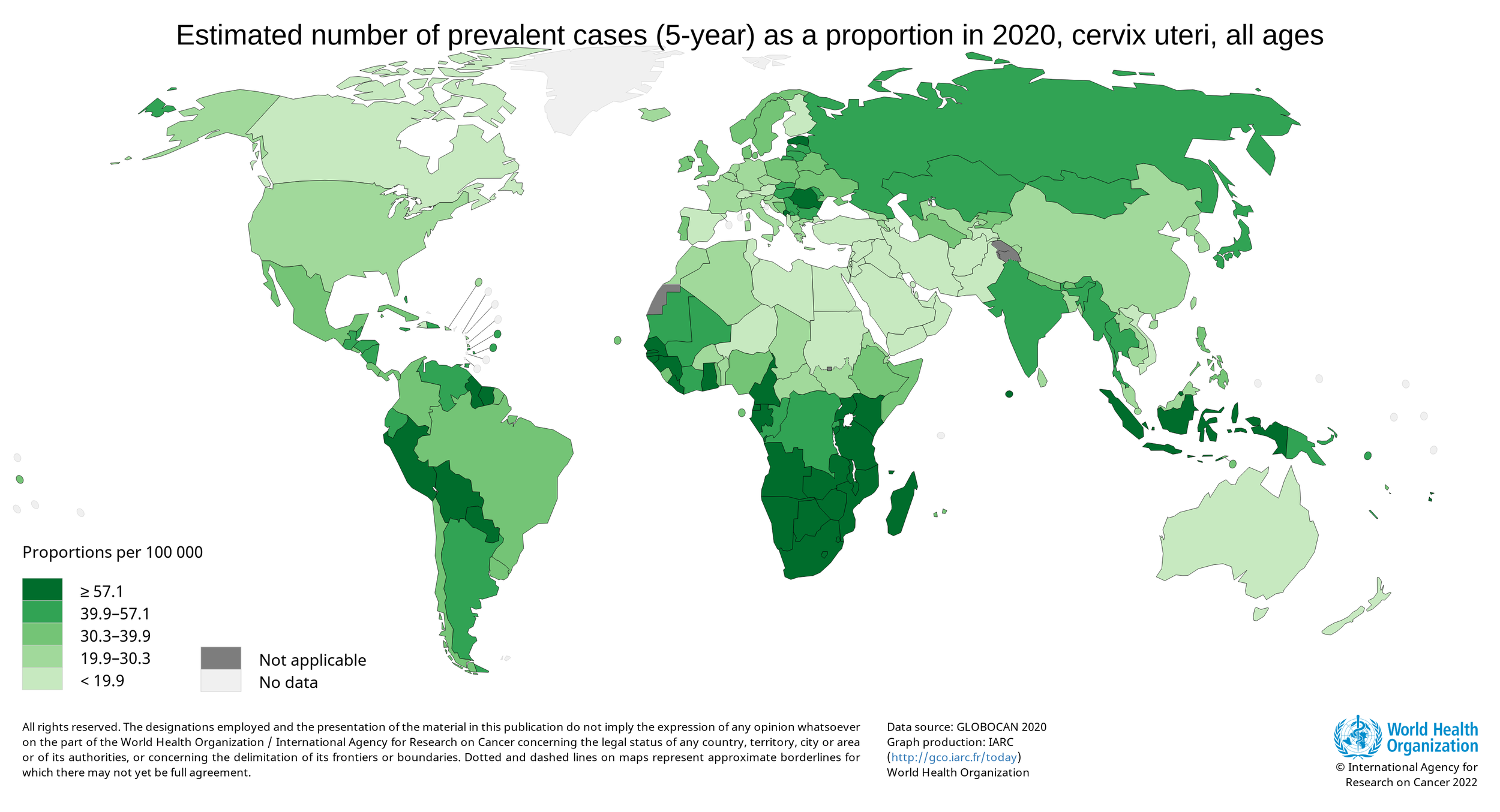
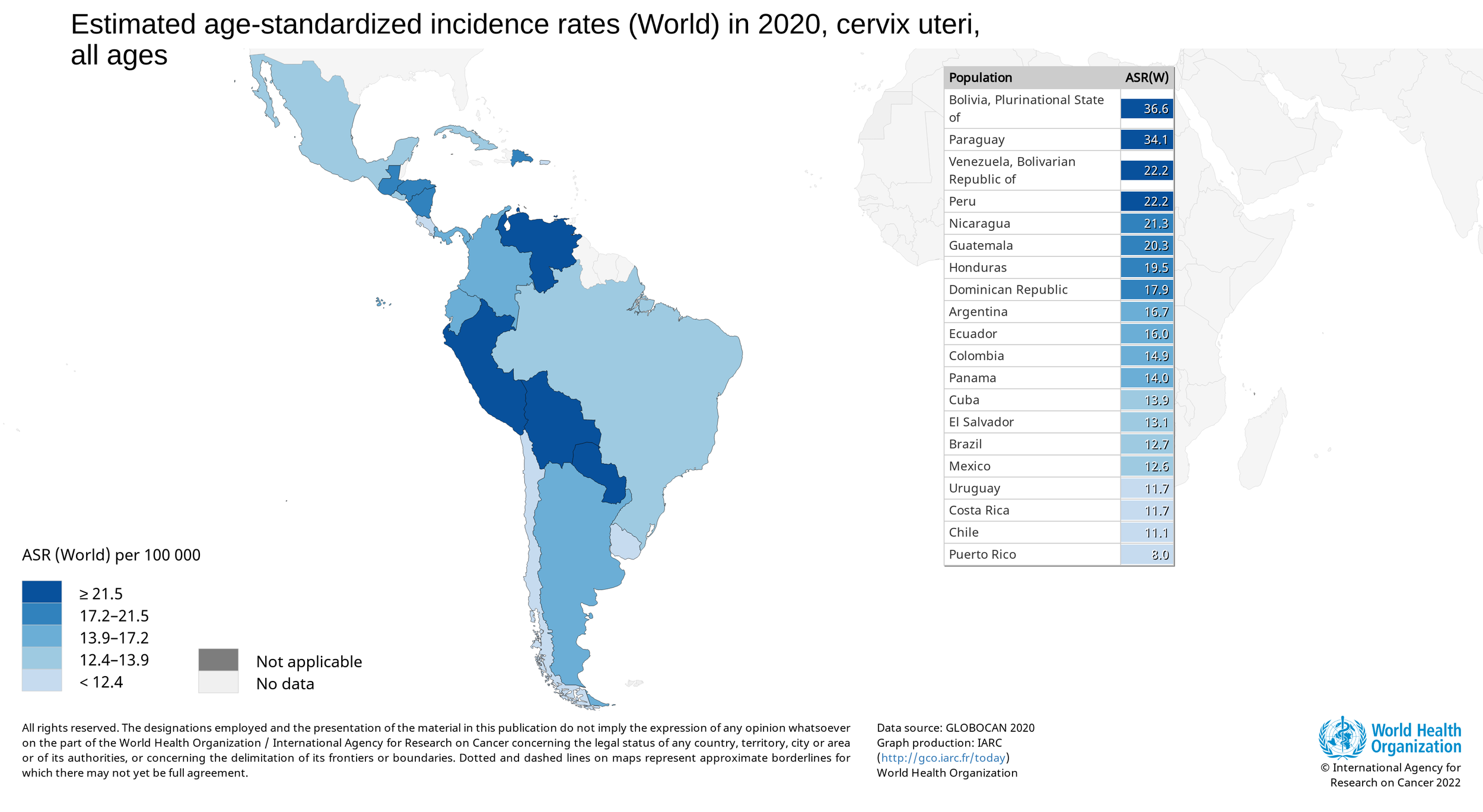
Yet over 56,000 new cases and 28,000 cervical cancer deaths occurred among women in Latin America
we asked why
During our team’s needs assessment trips over the years, local physicians and healthcare workers revealed that the most significant contributors to these high cervical cancer mortality rates were:
*click to drop down
-
Latin American nations have high rural-based populations, making mobile clinics a critical component for the delivery of health care. Mobile clinics often reached rural communities by trucks, on foot, and by horseback or ox. Dirt roads become hard to traverse depending on weather conditions such as rain or physical factors such as mountain slopes. Clinicians in these mobile units are limited in the equipment they could carry as well as their access to portable equipment overall.
-
Mobile clinics are often underfunded to conduct examinations in a private, safe, and efficient manner. A majority of financing for the Latin American health sector is dependent on other donation-based sources and some government aid. Through field interviews, clinics reported a variety of tools that could be used to perform their jobs more completely and efficiently, except that there was no money available to fund these changes.
Even with resources and increased screening access, it remains critical that tests performed are of quality and give accurate results. Mobile clinics resort to using makeshift surfaces, such as beds and tables, as examination tables, which impedes the clinician’s ability to accurately access the cervix. To ensure accuracy, Pap smears must access a specific region of cells on the cervix, which is moderately invasive. This area is a special transformation zone that contains specific mesothelial cells that are susceptible to HPV infection. Pap smears that are unable to access the lesion are a primary contributing factor to inaccurate test results.
-
Clinics revealed that they sometimes have to travel on foot, horseback, or ox to reach certain communities where there are not paved roads or pathways that allow motor vehicles to reach them. Dirt roads and mountainous terrain become hard to traverse depending on weather conditions such as rain and extreme heat.
Women in rural areas also face personal travel barriers. If a temporary clinic did not come directly to the rural community they reside in, the women would have to travel to the clinic on foot, bringing along any young children who cannot be left alone at home.
-
Cultural and education barriers often influence health outcomes as they pertain to women’s health in Latin American countries. Social expectations requiring mothers to stay at home and take care of the family, couples with need for additional family members to work and earn sustainable wages elicit a wide variety of barriers that can dissuade women from prioritizing their own health. This makes it even more imperative that exams are made as accessible as possible.
After conducting semi-structured interviews with women in Nicaragua, we found that the most prevalent concern was the intimacy of the screening. Women have reported feeling discomfort in receiving examinations in homes due to a lack of legitimacy in the exam process.
















































































































